Medical Reimbursement Consultants since 1985, (877) DON-SELF (877 366-7353)
2023 E&M Changes Full 1 Hour Webinar
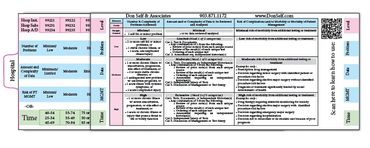
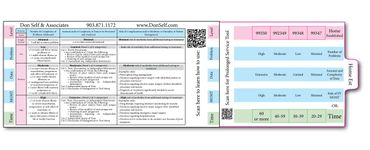
2023 brings the 2021 E&M rules to ALL PLACES OF SERVICE. This means the 95/97 rules are thrown out the window, along with the deletion of certain codes. This is great news and should save medical providers a ton of time.
This Non-CEU version of the webinar will cover the new coding rules. This includes:
How to select the level of service based on MDM or Time
What code sets were deleted
The prolonged service codes that were added
Examples of how to determine MDM elements
and more...
FREE 9 MINUTE MINI VIDEO 20203=
This 9 minute video is to help medical providers, billers and coders see how easy it is to document the Medical Decision Making & Time in 2023. Yes - the 95/97 rules have been tossed out like spending limits in Congress.
Photo Gallery




Cookie Policy
This website uses cookies. By continuing to use this site, you accept our use of cookies.
